Driver training for mentors who have learners who are diagnosed with diabetes or are at a high risk of developing diabetes
Welcome to the Hypodrive learner driver mentor program. This session is aimed at providing you with valuable information about Diabetes Mellitus, the types of diabetes, the management and complications and the questions you need to ask prior to driving. And you are all aware of the devastating consequences of how low or high blood glucose levels can impair your learners’ ability to drive safely. I would like this session to be interactive, so please don’t hesitate to ask questions and if you feel that you can’t ask a question during the presentation please slip it on a piece of paper and hand it to one of the presenters.
What is Diabetes Mellitus?
- A chronic disease characterised by high blood glucose (sugar) levels
- Occurs when the pancreas is unable to produce enough insulin, or the body becomes resistant to insulin, or both.
(Department of Health and Ageing, 2011)
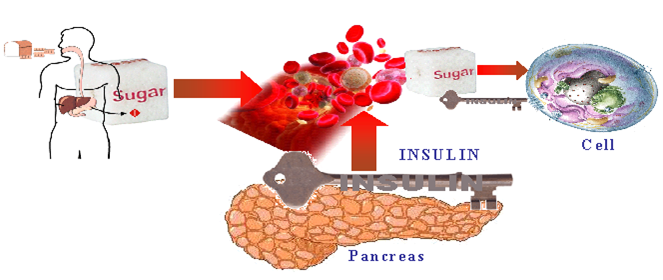
Where does the glucose come from?
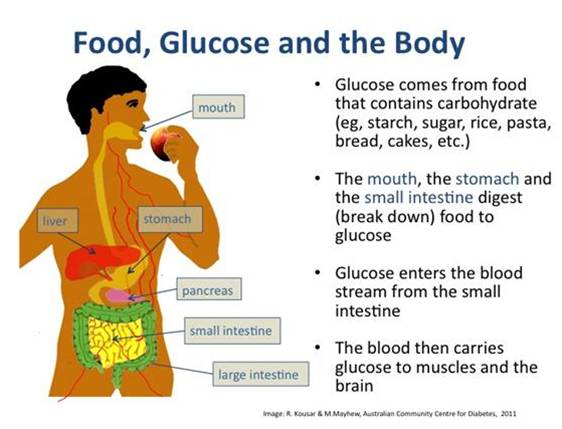
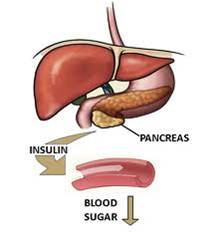
What is Insulin?
- Insulin is hormone made by the pancreas
- Acts like a key by unlocking the cell door (glucose channels) so that the sugar is moved from the blood stream into the muscles where we use it for energy
(Phillips, 2007, p. 11)
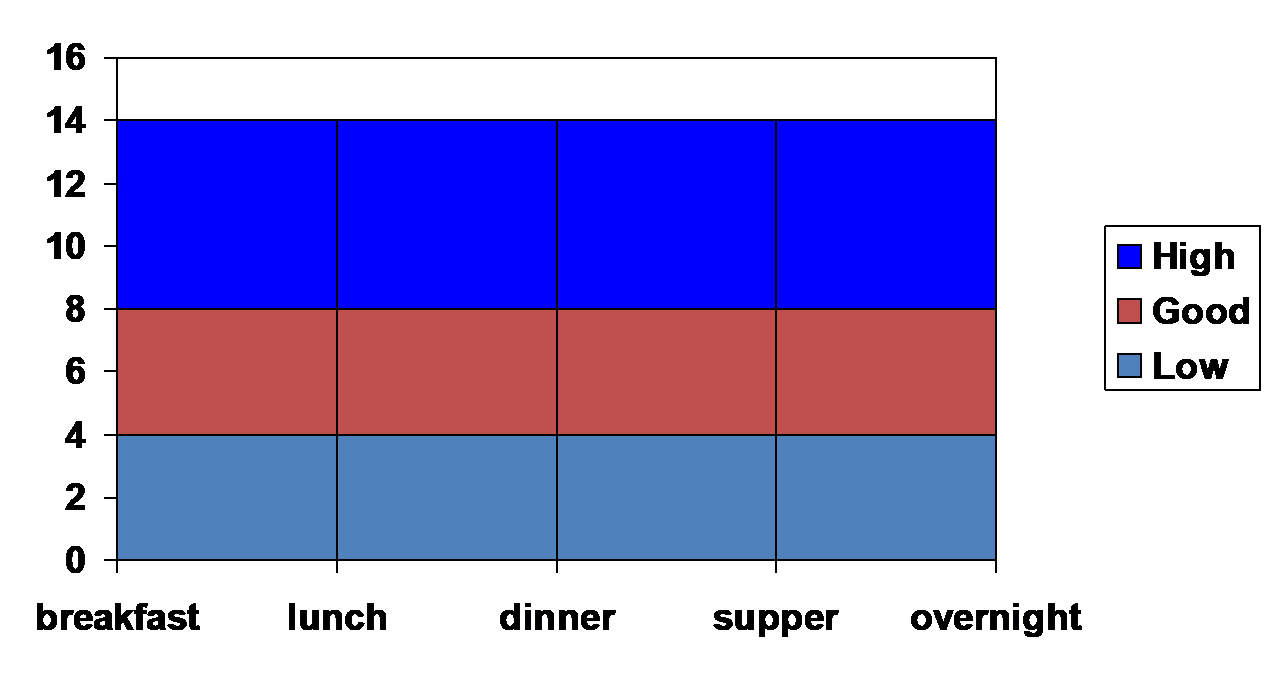
Glucose levels in response to eating
Source: National Diabetes Register and AIHW analysis of de-identified NDSS data (data extracted July 2011)
Until the age of 85 years, the incidence of insulin-treated Type 2 diabetes increased as people got older. For those aged 10–14 the incidence was 3 per 100,000 people and for the 55–69 year age group it was 238 per 100,000.
http://www.aihw.gov.au/diabetes/incidence/#t3
Diabetes – The Facts
- Diabetes has reached epidemic proportion in Australia and globally
- 1.7 million Australians have diabetes
- 275 diagnosed each day
- 60 a day in Queensland
(Department of Health and Ageing,, 2011 )
http://www.aihw.gov.au/publication-detail/?id=10737419311
What’s the concern?
- Increases the risk of heart attack and stroke
- Can lead to blindness
- Kidney failure
- Foot ulcers and amputation
- Impotence in men
- Affects driving ability
Healthinsite
– heart attacks and strokes: up to four times more likely in people with diabetes
– blindness: retinopathy affects one in six people with diabetes
– kidney damage: three times more common in people with diabetes
– amputations: 15 times more common in people with diabetes
Undetected or poorly controlled diabetes affects driving ability particularly if you are experiencing hyperglycaemia (high blood sugar) or hypoglycaemia (low blood sugar) it also increases the risk of long term complications which has a detrimental affect on your health.
Types of Diabetes
- Type 1 – 10-15% of the population
- Type 2 – previously accounts for 80-90% of people diagnosed with diabetes
- Gestational Diabetes (GDM)
(Bilous & Donnelly, 2010)
Type 2 Diabetes: Type 2 diabetes results from a combination of genetic and environmental factors and although there is a strong genetic predisposition, other risk factors include: ethnicity, increasing age, some medications (Steroids), and in some women, Polycystic ovarian syndrome (PCOS). Type 2 diabetes is a two step model first the body is resistant to insulin produced and over time it becomes deficient.
Gestational diabetes occurs in pregnancy and usually disappears when the baby is born, however, it can increase the risk of type 2 diabetes developing in women. (Diabetes Australia). (Diabetes Australia)
Diagnosis
- Ask your self am I at risk?
- http://www.health.gov.au/internet/main/publishing.nsf/Content/diabetesRiskAssessmentTool
- Fasting Blood Glucose test
- Oral glucose tolerance test (OGTT)
(Diabetes Management in General Practice 2011/2012)
On the other hand, the diagnosis of type 2 diabetes is determined by a three-step screening procedure, Firstly the initial risk assessment using a risk assessment tool or risk factors. The risk assessment tool is in your handouts please complete it and if you score high make an appointment to see your GP or feel free to talk to me after this session. Remember in most cases diabetes can be prevented and managed well.
Secondly – your GP will order a fasting blood test, this may also include cholesterol- if fasting 5.5-6.9mmol/L diabetes is uncertain Your GP will order a Oral Glucose Tolerance Test, this requires you to book into a pathology centre, you attend in the fasting state blood is taken and then you have to consume 75gms of glucose, 1 hour blood is taken again and at 2 hours. If fasting is greater than 7mmol/L or greater than or equal to 11.0mmol/L diabetes is likely. Diabetes Management in General Practice 2011/2012 pg.9
Management
 Healthy Eating
Healthy Eating- Regular Physical activity
- Blood glucose monitoring
- Medication and Insulin
- Regular check ups with health professionals
- Check daily foot wear
- Eye checks
- Dental checks
Ideal Blood Glucose Targets
- 4-6mmol/L fasting
- Up to 8mmol/L 2hours post meal
- 6-7mmol/L at bedtime
- Always Remember ‘5mmol/L or greater to drive’
It’s important that people with diabetes stabilise their blood glucose levels. What is termed ‘acceptable’ blood glucose levels can vary slightly but, as a general rule of thumb, fasting blood glucose levels should be less than 6.0 mmol/L, while non-fasting levels should be 4-8 mmol/L. If you plan on driving you should be 5mmol/L or greater before you drive and if you have a history of hypo unawareness you should be 6 or greater to drive.
As mentioned before by keeping your blood glucose as close as possible to normal reduces the risk of long-term complications of diabetes.
Acute Complications of Diabetes
- Hypoglycaemia (hypo)
- Hyperglycaemia (Hyper)
Hypoglycaemia (meaning low) commonly referred to as Hypo is classified when your blood glucose level falls below 4mmol/L or less with or with out symptoms.
Hyperglycaemia (meaning high) on the other hand is recognised when BGL’s are greater than 15mmol/L.
Hypoglycaemia (hypo’s)
- Defined as a blood glucose level <4mmol/L with or without symptoms
- Occurs in the people with diabetes treated with insulin and oral antidiabetic drugs (sulphonlyureas)
(Bilous& Donnelly,2010 )
So we need to ask who is at risk of a hypo? Firstly people at risk of a hypo are those taking insulin and people who are on certain oral medications for their diabetes. (Mathur, R)
Causes of Hypoglycaemia
- Insufficient carbohydrates
- Too much medication
- Too much physical activity
- Alcohol, up to 24 hours later
Signs and Symptoms
- Headache
- Hypothermia
- Visual Disturbances
- Mental Dullness
- Confusion
- Amnesia
- Seizures
- Coma
(Bilous& Donnelly, 2010)
Anyone who has experienced an episode of hypoglycaemia describes a sense of urgency to eat, which soon resolves the symptoms. And, that’s exactly the point of these symptoms. They act as warning signs. At this level, the brain still can access circulating blood glucose for fuel. The symptoms provide a person the opportunity to raise blood glucose levels before the brain is affected. (Mathur, R)
http://www.medicinenet.com/hypoglycemia/page2.htm
Signs and Symptoms
Neuroglucopenic
- Headache
- Hypothermia
- Visual Disturbances
- Mental Dullness
- Confusion
- Amnesia
- Seizures
- Coma
If not rising repeat step one
Step 2:
Give a long-acting carbohydrate
e.g: ½ sandwich
Or 2 to 4 dry biscuits
Or piece of fruit
Or glass of milk or tub of yoghurt
Hyperglycaemia
- Elevated blood glucose level (BGL) >15mmol/L due to a relative or absolute insulin deficiency
- Symptoms usually occur if BGL is persistently >15mmol/L
- Diabetic ketoacidosis (DKA) – Type 1
- Hyperosmolar coma – Type 2
- Chronic hyperglycaemia = defects in psychomotor tasks, attention, learning and memory
(Bilous & Donnelly, )
The cause of hyperglycaemia should be sought as soon as possible.
Most common causes are not enough medication or missing a dose of medication for the treatment of diabetes, including emotional Stress, pain, some medications such as cortisone, illness such as Infection, changes in food, reduced physical activity or a new diagnosis of Diabetes
Symptoms of Hyper’s
- Blood sugar levels greater than 15mmol/L
- Excessive thirst
- Increased urination
- Nocturia
- Fatigue
- Weight Loss
- Blurred vision
- Impaired cognitive function
- Change in behavior (usually irritable)
Management of hyperglycemia requires
Review of:
-Medication
-Diet
-Physical activity
-Stress
-Infection
Always Remember ‘5 to DRIVE’

References
fAustralianDemographic Statistics. http://www.oesr.qld.gov.au/products/briefs/aust-demographic-stats/qld-pop-counter.php
Bilous. R & Donnelly, R. 2010. Handbook of Diabetes. 4thedu. Wiley-Blackwell.
Betterhealth channel. Diabetes and coma http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Diabetes_and_coma
Diabetes in the Workplace http://www.diabetesvic.org.au/living-with-diabetes/diabetes-in-the-workplace
Glucagon Emergency Kit
http://www.drugs.com/cons/glucagon-emergency-kit.html
Diabetes Australia http://www.diabetesaustralia.com.au/en/Understanding-Diabetes/What-is-Diabetes/
Diabetes Facts http://www.diabetesvic.org.au/health-professionals/diabetes-facts
Driving and Diabetes http://www.diabetesvic.org.au/living-with-diabetes/driving-and-diabetes
Diabetes Management in General Practice, Guidelines for Type 2 Diabetes (2011/2012) p9.
Ian Goodall, Mark Shephardand Jill Tate: Recommended Changes in HbA1c Reporting Units for Australian Laboratories , Positon Statement of the Australasian Association of Clinical Biochemists http://www.aacb.asn.au/admin/?getfile=2802
Health insite – http://www.healthinsite.gov.au/topics/Diabetes
Mathur. R. Hypoglycaemia. http://www.medicinenet.com/hypoglycemia/page2.htm
Department of health and ageing: http://www.health.gov.au/internet/main/publishing.nsf/Content/pq-diabetes
My dr dot.com. Diabetes: monitoring and treating http://www.mydr.com.au/diabetes/diabetes-monitoring-and-treating
Phillips. P. Princeton (2007) Healthworks Blood Glucose. Princeton , Australia
Australian Institute of Health and Welfare http://www.aihw.gov.au/publication-detail/?id=10737419311
Australian Institute of Health and Welfare ,The incidence of insulin –treated type 2 diabetes http://www.aihw.gov.au/diabetes/incidence/#t3