Diabetes
Welcome to the Diabetes Component of Hypodrive. This session is aimed at providing you with valuable information about Diabetes Mellitus, the types of diabetes, the management and complications. And from theprevious presentation, we have heard of the devastating consequences of how low or high blood glucose levels can impair your or significant others ability to drive safely. I would like this to be interactive so please don’t hesitate to ask questions and if you feel that you can’t ask a question during the presentation please slip it on a piece of paper and hand it to one of the presenters.
The Facts
- Diabetes has reached epidemic proportion in Australia and globally
- 1.7 million Australians have diabetes
- 275 diagnosed each day
- 60 a day in Queensland
Department of health and ageing
Diabetes has reached epidemic proportion Globally. It is estimated that 1.7 million Australians have diabetes and half of these people don’t know they have it. (type 2 diabetes). And Type 2 diabetes continues to be the fastest growing chronic disease The 2007-08 Australian National Health Survey estimated that 4% of the population, have diabetes keeping in mind that this this survey relies on self-reported data. These figures have doubled since 1995 and In QLD there are approximately 300,000 people diagnosed with diabetes (Diabetes Australia QLD). It is estimated that two million Australians have pre-diabetes this putting them at risk of developing type 2 diabetes. Diabetes is the sixth leading cause of death in Australia
http://www.aihw.gov.au/publication-detail/?id=10737419311
Note: Excludes those aged less than 10 years.
Source: National Diabetes Register and AIHW analysis of de-identified NDSS data (data extracted July 2011)
This graph presents the latest statistics for people with type 2 diabetes using insulin. It needs to be noted that not all people with Type 2 diabetes need insulin for treatment and lifestyle modifications such as regular exercise and a healthy diet, along with medication. However some people require for insulin and this can depend on the duration of diabetes and the age. From 2000 to 2009, there were 94,663 males and 77,583 females who began to use insulin to treat their Type 2 diabetes. The average annual rate of new cases over this period was 95 per 100,000 people. This was 108 new cases per 100,000 for males and 82 new cases per 100,000 for females.
Until the age of 85 years, the incidence of insulin-treated Type 2 diabetes increased as people got older. For those aged 10–14 the incidence was 3 per 100,000 people and for the 55–69 year age group it was 238 per 100,000.
http://www.aihw.gov.au/diabetes/incidence/#t3
So Why The Concern?
Undetected or poorly controlled diabetes
- Increases the risk of heart attack and stroke
- Can lead to blindness
- Kidney failure
- Foot ulcers and amputation
- Impotence in men
- Affects driving ability
Healthinsite
Long term complications include:
– heart attacks and strokes: up to four times more likely in people with diabetes
– blindness: retinopathy affects one in six people with diabetes
– kidney damage: three times more common in people with diabetes
– amputations: 15 times more common in people with diabetes
Undetected or poorly controlled diabetes affects driving ability particularly if you are experiencing hyperglycaemia (high blood sugar) or hypoglycaemia (low blood sugar) it also increases the risk of long term complications which has a detrimental affect on your health.
What is Diabetes Mellitus?
- is a chronic disease characterised by high blood glucose (sugar) levels
- occurs when the pancreas is unable to produce enough insulin, or the body becomes resistant to insulin, or both.
Department of health and ageing
Diabetes comes from the Greek word meaning siphon as the body acts as a conduit for the excess fluid and Mellitus from the Greek and Latin work meaning honey. It is not a new disease as it is mentioned in ancient Egyptian era where they had water tasters. These people would taste the urine to check for diabetes. Not a good job to have I am sure. Today it is often simply referred to as diabetes and it is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin (insulin resistance). Blood sugar levels are controlled by insulin, a hormone produced by the pancreas and diabetes occurs when the pancreas is unable to produce enough insulin, or the body becomes resistant to insulin, or both.
Where does the glucose come from?
- Glucose is our main source of energy
- When eaten carbohydrates are broken down into glucose (sugar) where it is absorbed into the bloodstream.
- comes from carbohydrate foods such as bread, cakes, biscuits, pasta, rice, fruit, milk, yoghurt, potato and corn.
Link to animation- http://www.mydr.com.au/diabetes/animation-type-2-diabetes
Diabetes Australia
So where does the glucose in blood stream come from? Glucose comes from our main fuel source- “carbohydrates” and when we consume carbohydrates they are broken down into glucose where it is absorbed into the blood stream. Carbohydrates include all dairy products except for cheese (as when cheese is processed the sugar content is removed0, Legumes, Fruit, cereals, pasta, bread, and starchy vegetables. So you might say what can I eat, firstly lets not panic, to start off with there is nothing that you can’t eat, its just a matter of looking at serving sizes. At the same time it is important that we have sufficient carbohydrates each day as it is fuel for our bodies and if you want to think of our bodies as cars if we don’t have sufficient fuel we don’t function and nor would our car.
What is insulin?
- Insulin is hormone made by the pancreas
- acts like a key by unlocking the cell door (glucose channels) so that the sugar is moved from the blood stream into the muscles where we use it for energy
Phillips pg 11
Insulin is a hormone produced by the beta cells in the pancreas and its function is to helps transfer glucose from the blood stream into the cell
So in other words think of insulin like a key to unlock the cell doors (glucose channels) in the body’s cells so that glucose can enter the cells and be used for energy. So in effect insulin helps the body remove glucose from the blood stream and helps keep the levels of blood glucose stable. (Phillips, P. Princeton Health works)
Glucose levels in response to eating
In response to carbohydrate intake your blood glucose and insulin levels will fluctuate and in a person without diabetes normal blood glucose levels range from 3-8.0mmol/L (Phillips pg11)
Types of Diabetes
- Type 1- 10-15% of the population
- Type 2-previously accounts for 80-90% of people diagnosed with diabetes
- Gestational Diabetes (GDM)
Bilous& Donnelly
Type 1 diabetes is an auto-immune disease in which the body’s immune system destroys the insulin-producing beta cells in the pancreas. This type of diabetes, also known as juvenile-onset or insulin-dependent diabetes, accounts for 10-15% of all people with the disease. Usually develops rapidly and it can appear at any age (usually children), although commonly under 40, and is triggered by environmental factors such as viruses, diet or chemicals in people genetically predisposed. People with type 1 diabetes must inject themselves with insulin several times a day and follow a healthy diet and exercise plan. In other words they have to think like a pancreas.
Healthinsite type 1 diabetes.
Type 2 Diabetes:Type 2 diabetes results from a combination of genetic and environmental factors and although there is a strong genetic predisposition, other risk factors include: ethnicity,increasing age, some medications (Steroids), and in some women Polycystic ovarian syndrome (PCOS) and finally Gestational Diabetes. Gestational diabetes occurs in pregnancy and usually disappears when the baby is born, increases the risk of type 2 diabetes in women.(Diabetes Australia). Type 2 diabetes is a two step model first the body is resistant to insulin produced and over time it becomes deficient. (Diabetes Australia)
Symptoms of Diabetes
- Blurred vision;
- Tiredness;
- Urinating more frequently;
- Feeling thirsty all the time;
- Numbness and tingling in the feet or legs; and
- Recurrent infections.
Healthiinsite
Symptoms forType 1 usually occur rapidly where for type 2 there is a gradual onset. If these symptoms occur, you should see a doctor. More importantly it is advisable to have regular health checks. Most of you have your cars serviced on a regular basis, you change the oil so why not give you body the service that it needs. Every year have a health check from your GP or I usually call it my 50,000 km service!! (Health insite)
Diagnosis
- Ask your self am I at risk?
- http://www.health.gov.au/internet/main/publishing.nsf/Content/diabetesRiskAssessmentTool
- Fasting Blood Glucose test
- Oral glucose tolerance test (OGTT)
Diabetes Management in General Practice 2011/2012
The diagnosis of type 1 diabetes is usually clear cut the person presents with weight loss, increased thirst and having to go to the toilet frequently, blurred vision and with or with out vomiting and abdominal pain.
On the other hand the diagnosis of type 2 diabetes is determined by a three-step screening procedure, Firstly the initial risk assessment using a risk assessment tool or risk factors. The risk assessment tool is in your handouts please complete it and if you score high make an appointment to see your GP or feel free to talk to me after this session. Remember in most cases diabetes can be prevented and managed well.
Secondly – your GP will order a fasting blood test, this may also include cholesterol- if fasting 5.5-6.9mmol/L diabetes is uncertain Your GP will order a Oral Glucose Tolerance Test, this requires you to book into a pathology centre, you attend in the fasting state blood is taken and then you have to consume 75gms of glucose, 1 hour blood is taken again and at 2 hours. If fasting is greater than 7mmol/L or greater than or equal to 11.0mmol/L diabetes is likely. Diabetes Management in General Practice 2011/2012 pg.9
Answer the following questions
Remember to keep a record of your score as you go.
Your age group
Under 35 years – 0 points
35 – 44 years – 2 points
45 – 54 years – 4 points
55 – 64 years – 6 points
65 years or over – 8 points
Your gender
Female – 0 points
Male – 3 points
Your ethnicity/country of birth:
Are you of Aboriginal, Torres Strait Islander, Pacific Islander or Maori descent?
No – 0 points
Yes – 2 points
Where were you born?
Australia – 0 points
Asia (including the Indian sub-continent), Middle East, North Africa, Southern Europe – 2 points
Other – 0 points
Have either of your parents, or any of your brothers or sisters been diagnosed with diabetes (type 1 or type 2)?
No – 0 points
Yes – 3 points
Have you ever been found to have high blood glucose (sugar) (for example, in a health examination, during an illness, during pregnancy)?
No – 0 points
Yes – 6 points
Are you currently taking medication for high blood pressure?
No – 0 points
Yes – 2 points
Do you currently smoke cigarettes or any other tobacco products on a daily basis?
No – 0 points
Yes – 2 points
How often do you eat vegetables or fruit?
Every day – 0 points
Not every day – 1 point
On average, would you say you do at least 2.5 hours of physical activity per week (for example, 30 minutes a day on 5 or more days a week)?
Yes – 0 points
No – 2 points
Your waist measurement taken below the ribs (usually at the level of the navel, and while standing)
The correct place to measure your waist is halfway between your lowest rib and the top of your hipbone, roughly in line with your navel. Measure directly against your skin, breathe out normally, make sure the tape is snug, without compressing the skin. Make a note of your waist measurement and score as below.
For those of Asian or Aboriginal or Torres Strait Islander descent:
Men
Less than 90 cm – 0 points
90 – 100 cm – 4 points
More than 100 cm – 7 points
Women
Less than 80 cm – 0 points
80 – 90 cm – 4 points
More than 90 cm – 7 points
For all others (i.e. not of Asian or Aboriginal or Torres Strait Islander descent:)
Men
Less than 102 cm – 0 points
102 – 110 cm – 4 points
More than 110 cm – 7 points
Women
Less than 88 cm – 0 points
88 – 100 cm – 4 points
More than 100 cm – 7 points
Your risk of developing type 2 diabetes within 5 years*
Check your total score against the three possible point ranges below.
5 or less: Low risk
If you scored 5 or less you are at low risk of developing type 2 diabetes within 5 years – approximately one person in every 100 will develop type 2 diabetes.
6 – 11: Intermediate risk
If you scored 6 to 11 you are at intermediate risk of developing type 2 diabetes within 5 years – for scores of 6 to 8, approximately one person in every 50 will develop diabetes. For scores of 9-11, approximately one person in every 30 will develop diabetes. Print this form and take it to your doctor. Discuss with the doctor your score and your individual risk. Improving your lifestyle may help reduce your risk of developing type 2 diabetes.
12 or more: High risk
If you scored 12 or more you are at high risk of developing type 2 diabetes within 5 years or you may have undiagnosed type 2 diabetes. For scores of 12-15, approximately one person in every 14 will develop diabetes. For scores of 16 to 19, approximately one person in every 7 will develop diabetes. For scores of 20 and above, approximately one person in every 3 will develop diabetes. Print this form and take it to your doctor. Ask your doctor about having a fasting blood glucose test. Act now to prevent type 2 diabetes.
Management
- Healthy Eating
- Regular Physical activity
- Blood glucose monitoring
- Medication and Insulin
- Regular check ups with health professionals
- Check feet daily wear appropriate foot wear
- Eye checks
- Dental
Living well with diabetes means keeping blood glucose level as close to normal range as possible.(Health insite). And the biggest problem with diabetes is that elevated BGL’s produce no pain, so people are not inclined to go to the doctor as much as they would if they had an ache that never went away. As a diabetes educator I am continually informing people of the problems associated with elevated readings but its hard for people to into consideration because they haven’t got a problem with their eyes, feets etc so why should I change. I ask you to think what would you do?? Are you going to make a change that will have an impact on your life or say well when it happens then I will deal with it. Well its your choice but if you change your eating habits to a healthier version even if its one thing you are on the way. It is important to maintain healthy eating andthis will be discussed in the next session at the same time aim for at least 30 minutes of physical activity and this will also be in the activity component. Start thinking of ways that you can get more physical activity in your day. For example take the stairs instead of the elevator. Use the broom instead of the blower, get up and change the channels. Additionally it is important to have regular check ups with health professionals such as regular blood tests, monitoring HbA1C. checking blood pressure, cholesterol levels, checking feet.
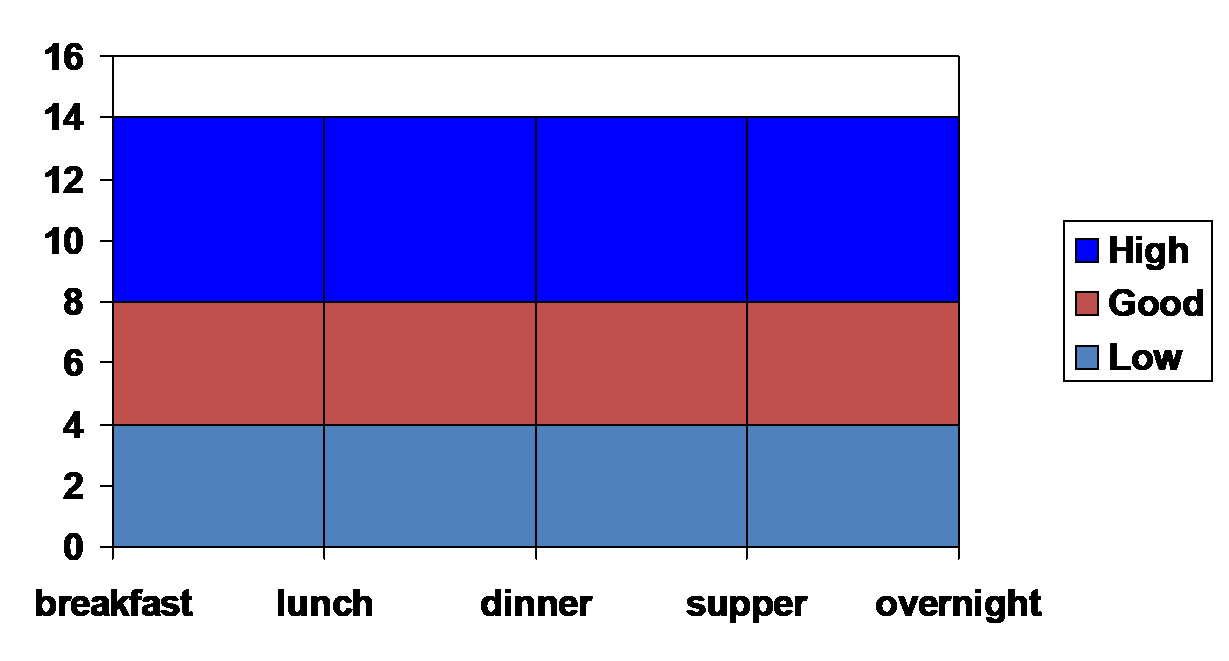
Ideal Blood Glucose Targets
- 4-6mmol/L fasting
- Up to 8mmol/L 2hours post meal
- 6-7mmol/L at bedtime
- Remember 5mmol/L or greater to drive
So what is your target blood sugar level? Well for starters it depends on many factors, including whether you have type 1 or type 2 diabetes mellitus, your age, overall health, social support system and personal preferences.
It’s important that people with diabetes stabilise their blood glucose levels. What is termed ‘acceptable’ blood glucose levels can vary slightly but, as a general rule of thumb, fasting blood glucose levels should be less than 6.0 mmol/L, while non-fasting levels should be 4-8 mmol/L. If you plan on driving you should be 5mmol/L or greater before you drive and if you have a history of hypo unawareness you should be 6 or greater to drive.
As mentioned before by keeping your blood glucose as close as possible to normal reduces the risk of long-term complications of diabetes.
Acute complications of diabetes
occur if diabetic management is not optimal
- Hypoglycaemia (hypo)
- Hyperglycaemia (Hyper)
There are two acute complications of diabetes this meaning that they can occur quickly and at intervals and in most cases they are often preventable.
Hypoglycaemia (meaning low) commonly referred to as Hypo is classified when your blood glucose level falls below 4mmol/L or less with or with out symptoms.
Hyperglycaemia (meaning high) on the other hand is recognised when BGL’s are greater than 15mmol/L.
Hypoglycaemia (hypo’s)
- Defined as a blood glucose level <4mmol/L with or without symptoms
- Occurs in the people with diabetes treated with insulin and oral antidiabetic drugs (sulphonlyureas)
Bilous& Donnelly
Symptoms of hypoglycaemia can vary from person to person, as can the severity. Classically, hypoglycaemia is diagnosed by a low blood sugar of 4mmol/L or less and in some instances with or without symptoms. The brain cannot make its own glucose and is 100% dependent on the rest of the body for its supply. In fact in order to function the brain requires 120-140g glucose per day (demonstrate what this is by a food model). In the event that the brain’s requirements increase and/or the demands are not met the glucose level in the blood falls resulting in decreased cognitive function.
So we need to ask who is at risk of a hypo? Firstly people at risk of a hypo are those taking insulin and people who are on certain oral medications for their diabetes. (Mathur, R)
Causes of Hypoglycaemia
– insufficient carbohydrates
– too much medication
– too much physical activity
– alcohol up to 24 hours later
There are several factors that can contribute to a hypo and they can be caused by too much insulin or oral medication,
Insufficient carbohydrates, a delayed or missed meal or snack
Increased physical activity either intentional or unintentional.
Or alcohol is consumed without eating food or on the other hand too much alcohol is consumed. When people consume alcohol their levels may be elevated to begin with but the liver needs to get rid of the alcohol as it is a toxin so it stops the normal production of glucose to break down the alcohol. People on insulin and some oral medications are at risk of a hypo up to 24 hours after they have consumed it. (Betterhealth channel)
Signs and Symptoms
Sympathetic
– Hunger
– Weakness
– Sweating
– Tachycardia
– Palpitations
– Tremor
– Nervousness
– Irritability
– Tingling of mouth and fingers
Bilous& Donnelly
The first set of symptoms are called sympathetic (or adrenergic) because they relate to the nervous system’s response to hypoglycaemia and for a majority of people, these symptoms are easily recognizable. They may experience symptoms, Hunger,Weakness,Sweating,Tachycardia,Palpitations,Tremor,Nervousness, Irritability,Tingling of mouth and fingers
Anyone who has experienced an episode of hypoglycaemia describes a sense of urgency to eat and resolve the symptoms. And, that’s exactly the point of these symptoms. They act as warning signs. At this level, the brain still can access circulating blood glucose for fuel. The symptoms provide a person the opportunity to raise blood glucose levels before the brain is affected. (Mathur, R)
http://www.medicinenet.com/hypoglycemia/page2.htm
Neuroglucopenic
-Headache
-Hypothermia
-Visual Disturbances
-Mental Dullness
-Confusion
-Amnesia
-Seizures
-Coma
In the event that the person does not or cannot respond by eating something to raise blood glucose, the levels of glucose continue to drop. Most will progress to neuro-glyco-penic symptoms (the brain is not getting enough glucose). At this point, symptoms progress to confusion, drowsiness, changes in behavior, coma, and seizure. (Mathur, R)
Treatment Hypoglyceamia
Rapid treatment is important
Step 1:
-Test and record BGL
-Give quick-acting sugar/glucose to raise the BGL
e.g: 3 level teaspoons of sugar or honey or 6-7 jelly beans
Or 1 cup of orange juice or soft drink (not diet)
Or glucose preparation (glucose gel/tablets)
In the event that you have symptoms of a hypo or your blood glucose level is 4mmol/L or less rapid treatment is crucial, consume 15 grams of glucose or rapid acting carbohydrate,followed by an assessment of symptoms and a blood glucose check if possible after 10-15 minutes if the BGL is not rising give another 15 grams of rapid acting glucose. This can be repeated up to three times. At that point, the individual should be considered as not responding to the therapy and an ambulance should be called. (Mathur, R). If driving immediately pull over to side of the road, turn the engine off remove car keys and put hazard lights on and use the contents of your hypodrivehypokit.
?The ability to drive has been shown to be impaired when blood glucose levels fall below 5mmol/L. http://www.diabetesvic.org.au/living-with-diabetes/diabetes-in-the-workplace
Check BGL 10-15 minutes later to ensure it is rising
If not rising repeat step one
Step 2:
Give a long-acting carbohydrate
e.g: ½ sandwich
Or 2 to 4 dry biscuits
Or piece of fruit
Or glass of milk or tub of yoghurt
Always give a long acting or slow release carbohydrate once BGL is on the increase. It is advisableto wear identification stating they have diabetes and whether you have recurrent hypoglycaemia.. Always check blood sugars before they drive a car, operate heavy machinery, or do anything physically taxing. Remember must be 5 or greater to drive and if you have hypo unawareness then you should be 6mmol/L or greater to drive. Always carry a quick-acting glucose source (such as those mentioned) at all times, and keep the HYPODRIVE HYPO-KIT in your car, the office, and by their bedside. On a final note many people like the idea of treating hypo’s with cake, cookies, or chocolate. However, sugar in the form of complex carbohydrates or sugar combined with fat and protein are much too slowly absorbed to be useful in the acute treatment of hypoglycaemia. Save the chocolate for treats.
Glucagen hypo kit
- . It is an emergency medicine used to treat severe hypoglycemia (low blood sugar) in patients with diabetes who have passed out or cannot take some form of sugar by mouth.
Hyperglycaemia
Refers to an elevated blood glucose level >15mmol/L due to a relative or absolute insulin deficiency
- Symptoms usually occur if BGL is persistently >15mmol/L
- Diabetic ketoacidosis (DKA) – type 1
- Hyperosmolar coma – type 2
- Chronic hyperglycaemia = defects in psychomotor tasks, attention, learning and memory
Bilous& Donnelly
Hyperglycaemia refers to an elevated BGL of 15mmol/l or greater and chronic or continual elevation in BGL’s affects the individual’s to function.
The cause of hyperglycaemia should be sought as soon as possible.
Most common causes are not enough medication or missing a dose of medication for the treatment of diabetes
Emotional Stress
Pain
Some medications such as cortisone
Illness such as Infection
Changes in food
Reduced physical activity
New diagnosis of Diabetes
Symptoms
- Blood sugar levels greater than 15mmol/L
- Excessive thirst
- Urinating a lot
- Nocturia
- Fatigue
- Weight Loss
- Blurred vision
- Impaired cognitive function
- Change in behavior (usually irritable)
Symptoms include blurred vision (The blurred vision is a result of the lens of your eye changing shape which ultimately affects your ability to drive). (My Dr) Elevated BGL’s also contribute to Change in behavior (usually irritable) and Impaired cognitive functionall affecting judgment and the ability to drive appropriately. It is recommended that you don’t drive until your BGL’s are within range and/or the symptoms of hyper glycaemia have resolved.
Management of hyperglycemia requires
Review of:
-Medication
-Diet
-Physical activity
-Stress
-Infection
- Remember 5 to DRIVE
Question
- Can I be discriminated about my diabetes at work?
- Could I manage my diabetes so I don’t put the safety of other co-workers at risk
- How will I manage hypo’s at work?
- Am I able to check my BGL’s on a regular basis and have regular breaks
- Should I disclose my Diabetes to my employer or work colleagues?
- Seek advice first
While at work the biggest question that needs to be addressed is could I manage my diabetes so I don’t put the safety of myself and other of co-workers at risk for example if I fail to check my blood glucose levels and I experience a hypo could this cause injury or even death? On the other hand are my sugar levels high resulting in the inability to function and if we remember what some of the symptoms of elevated sugar levels are such as fatigue,Blurred vision,Impaired cognitive function,Change in behavior (usually irritable)
You need to be prepared and ask yourself how will I am going to manage my hypo’s at work, who do I tell that I have diabetes and if I am at risk of a hypo? Am I able to check my BGL’s on a regular basis and can I have regular meal breaks.
Your rights and responsibilities
- should disclose the fact that I have Diabetes?
- Diagnosis of diabetes may mean you have legal responsibility to notify the transport authority
- Do I have a responsibility to disclose my diabetes if my work involves driving or operating machinery
- Will I be discriminated against?
- Two types of discrimination
– Direct
– Indirect
The biggest question is whether you should disclose the fact that you have Diabetes to either your employer or work colleagues? For starters his is entirely up to you but remember the need for safety and the safety of others working with you. You need to address whether the medications that you are taking are likely to have side effects that may affect my work performance. Also consider what sort of work do you do, (say for example you are at risk of a hypo and you are required to climb onto roofs or confined spaces. Risk of falling or very hard to get you out.
What are the work cover and insurance disclosure requirements or if I have an accident or I am injured at work was it do to the management of my diabetes?
Once diagnosed with diabetes you have legal responsibility to notify the transport authority in your state. Question do I have a responsibility to disclose my diabetes? Yes if your work involves driving or operating machinery
or you drive a company car then you must disclose your diabetes to your employer.
Will I be discriminated against?
Often people with diabetes feel that they are being discriminated however there are laws to protect you against discrimination in the workplace
Under the Equal opportunity Act 1995 your employer has legal obligations and responsibilities
And when we look at discrimination there are two types
1). Direct is when someone is treated less favourably because of their diabetes- for example your job is terminated because of your diabetes
2). Indirect occurs when a workplace has requirements or practices that may appear fair but in fact discriminate against people on the basis of a particular characteristic such as not accommodating the need for regular meal breaks or somewhere you can check your BGL’s or inject your insulin
Develop and Action Plan
Describe you signs and symptoms and if having a hypo you might not be co-operative
inform co-workers when to call OOO
Have a hypo kit in the work place
Put ICE (in case of emergency) in your phone contacts
References
Assessing Fitness to drive for commercial and private vehicle drivers. http://www.austroads.com.au/images/stories/Assessing_Fitness_to_Drive_Small_Size.pd
fAustralianDemographic Statistics. http://www.oesr.qld.gov.au/products/briefs/aust-demographic-stats/qld-pop-counter.php
Bilous. R & Donnelly, R. 2010. Handbook of Diabetes. 4thedu. Wiley-Blackwell.
Betterhealth channel. Diabetes and coma http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Diabetes_and_coma
Diabetes in the Workplacehttp://www.diabetesvic.org.au/living-with-diabetes/diabetes-in-the-workplace
Glucagon Emergency Kit
http://www.drugs.com/cons/glucagon-emergency-kit.html
Diabetes Australia http://www.diabetesaustralia.com.au/en/Understanding-Diabetes/What-is-Diabetes/
Diabetes Factshttp://www.diabetesvic.org.au/health-professionals/diabetes-facts
Driving and Diabeteshttp://www.diabetesvic.org.au/living-with-diabetes/driving-and-diabetes
Diabetes Management in General Practice, Guidelines for Type 2 Diabetes (2011/2012) p9.
Ian Goodall, Mark Shephardand Jill Tate: Recommended Changes in HbA1c Reporting Units for Australian Laboratories , Positon Statement of the Australasian Association of Clinical Biochemists http://www.aacb.asn.au/admin/?getfile=2802
Health insite – http://www.healthinsite.gov.au/topics/Diabetes
Mathur. R. Hypoglycaemia. http://www.medicinenet.com/hypoglycemia/page2.htm
Department of health and ageing: http://www.health.gov.au/internet/main/publishing.nsf/Content/pq-diabetes
My dr dot.com. Diabetes: monitoring and treating http://www.mydr.com.au/diabetes/diabetes-monitoring-and-treating
Phillips. P. Princeton (2007) Healthworks Blood Glucose. Princeton , Australia
Australian Institute of Health and Welfare http://www.aihw.gov.au/publication-detail/?id=10737419311
Driving and diabetes
Important facts
- The safety of you and others on the road is the main concern.
- You must notify your state or territory licensing authority that you have diabetes.
- Driving a motor vehicle is a complex task involving perception, appropriate judgement, adequate response time and reasonable physical capability.
- Carry hypo treatment with you all the time if you are on medication or insulin.
Each year in Australia more than 1,500 Australians are killed on our roads and around 22,000 are seriously injured. The total economic cost of this exceeds $15 billion annually and the
accompanying social costs greatly impact on our communities. Therefore if you have diabetes there are some important facts that you need to know about driving.
Firstly you must notify your state or territory licensing authority that you have been diagnosed with diabetes or the management of your diabetes has changed.
Secondly Driving a motor vehicle is a complex task involving perception, appropriate judgement, adequate response time and reasonable physical capability and for people with diabetes, the ability to drive safely can be affected by:
Hypoglycaemia (low blood glucose level)
Hyperglycaemia (high blood glucose level)
Therefore, there are several precautions that you should take. If on certain oral medications or insulin you are at risk of hypoglycaemia therefore it is important that carry some form of hypo treatment with you.
(Assessing Fitness to drive for commercial and private vehicle drivers, 2006)
Other factors which can affect the ability to drive include Impaired vision from retinopathy, high blood glucose levels,Numb feet or hands (neuropathy)
Precautions when driving
- Check your blood glucose level before driving
- Do not drive unless over 5 mmol/L
- If you experience symptoms of a hypo while driving, immediately pull over and put hazard lights on turn off the car.
- Treat hypo as recommended
- Do not drive again until your blood glucose level returns to normal and you feel better
- Stop every 2 hours for long trips and check blood glucose level before driving again
- Wear identification
- If you have hypo unawareness you must be 6mmol/L or greater to drive.
Always check your blood glucose level before driving, Do not drive unless 5 mmol/L or greater and if you have a history of hypo unawareness you must be 6mmol/ L or greater.
Take your meter, hypo treatment (e.g. jelly beans) and carbohydrate snacks with you, even on short trips you just never now when you may get stuck in traffic or the car breaks down. In fact keep a kit in your car at all times. If you experience symptoms of a hypo while driving, immediately pull over and put hazard lights on turn off the car. Treat hypo as recommended
Do not drive again until your blood glucose level returns to normal and you feel better
For long trips plan regular stops, it is recommended that you stop every 2 hours, check your blood glucose levels
Wear identification that states your name, doctor and diabetes treatment
If you think you have hypo unawareness speak to your doctor or diabetes educator to take steps to regain your awareness again.
Your state or territory licensing authority has the responsibility to ensure all licence holders are fit to drive and the safety of you and others on the road is the main concern. Relevant legislation and procedures are not intended to deny an individual the right to hold a driver licence the main intent is to protect the safety of the community and the individual concerned.